|
 |
- Search
| J EMS Med > Volume 1(1); 2022 > Article |
|
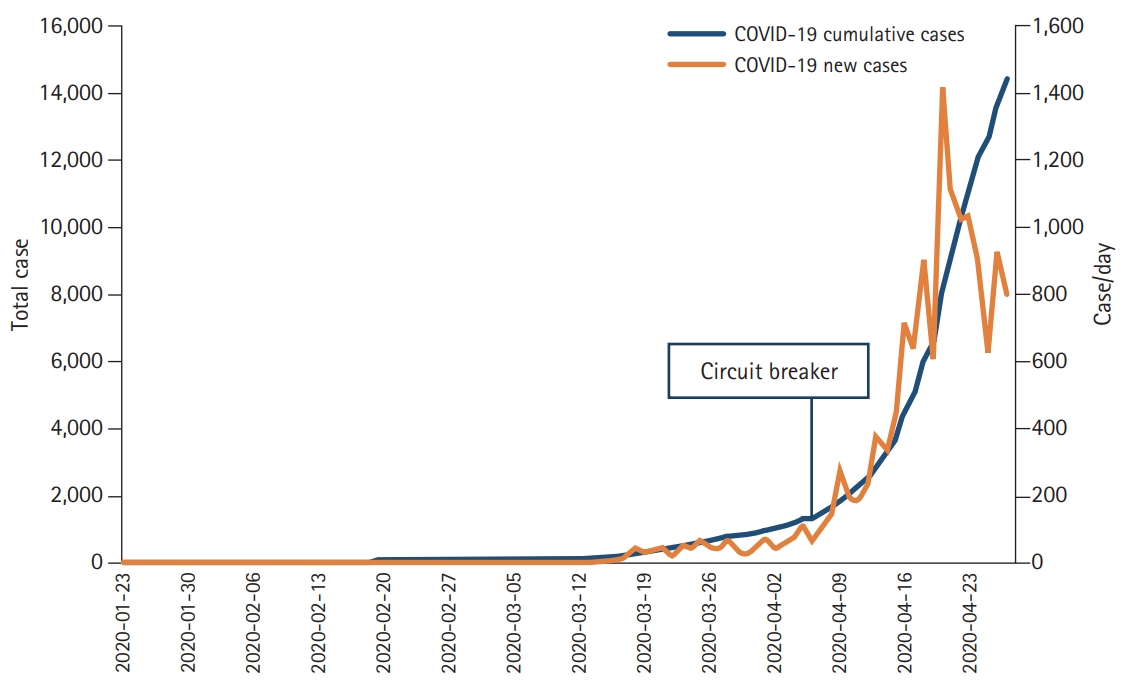
As we all know that Singapore reported its first corona virus disease 19 (COVID-19) case on January 23, 2020, just 2 months after the reporting of the first case in Wuhan [1]. For the next several weeks, newly identified cases per day hovered around ten arising from a few known clusters and business as usual continued until mid-March. However, the new cases increased to hundreds per day in the next 2 weeks. The increase was attributed to returning citizens/residents from overseas. This increase led to the implementation of preventive public health measures aiming at improving personal hygiene and maintaining physical distance at public venues and workplaces. Soon measures were further tightened as the number continued to rise. Cases among migrant workers living in dormitories started appearing. Anticipating an even sharper increase in new cases, the government enforced more extensive social distancing measures under the rubric of ‘circuit breaker’ on April 7, 2020. All social meetings/gatherings beyond household members were banned. All non-essential work places including educational and training institutes, social and religious gathering places were either shut down or staff was asked to work remotely, where possible. Only essential commodity retailers and critical services were allowed to operate with strict social distancing and viral transmission prevention measures. The number of new cases crossed 1,000 per day by the third week. As these lines are being written (May 2020), the circuit breaker is in effect, and the count is rising (Fig. 1).
Singapore’s response to the COVID-19 epidemic was influenced by its experience of the 2003 severe acute respiratory syndrome (SARS) outbreak [2]. A multi-agency response against COVID-19, bolstered by relevant laws, was swiftly put in place comprising of case detection, contact tracing followed by isolation and quarantine with concomitant management. Together, these initiatives led to a measured response that succeeded in obtaining public support and thus achieved the desired results [3,4].
However, COVID-19 proved to be very different from the SARS outbreak, more infectious with asymptomatic transmission but less lethal [5,6]. The rising number of cases despite stringent control measures, confinement of people in limited spaces, closure of businesses, and perceived uncertainty in the supply of essential goods have instilled a sense of uneasiness. Many are asking one fundamental question: how long will this epidemic last [7]? The question is also relevant to the health system. Our objective here is to portray some potential scenarios this epidemic may follow over the coming months or years in Singapore, and maybe in other geographies, priming the public and planners for appropriate preparations. Pathogen characteristics and transmission dynamics of SARS coronavirus 2 and other corona viruses have been considered while proposing these scenarios [8–10].
Scenario 1: A short-lived, single wave epidemic. It can be considered as the best-case or the most desirable scenario, where Singapore experiences a single ‘wave’ of cases reaching a peak in a short time, followed by a relatively slow decline. As strict social distancing measures are enforced, and multi-agency efforts in the dormitories to screen, test, isolate, and treat cases take effect, the number of cases starts to drop. Meanwhile, hospitals are stretched managing the load of the rising number of patients, especially the ones requiring high dependency care. Hospitals face a shortage of drugs and supplies, but are able to mobilize resources to cope with the surge. It is followed by a gradual decline in new cases, although a small number of cases continue to be identified for the next several months. No vaccine or drug can be approved. Extended border controls and travel restrictions minimize the chances of re-introduction of a new wave of infections. Globally, the pandemic starts waning, restrictions within and between countries are gradually eased out. Globally the death toll is significant. Economic activity slowly revives, and life returns to normal, though with caution and fear for most people (Fig. 2).
Scenario 2: A prolonged epidemic with several waves. Alternatively, after braving the first wave of the epidemic life returns to normalcy only for a second wave of imported cases to emerge, creating new clusters. With measures in place and comparatively fewer susceptible individuals, the second wave is slower to progress. However, it still prompts enforcement of another instance of social distancing measures. The cycle may repeat with an increasing gap between consecutive waves but resulting in fewer cases and deaths each time. Eventually, vaccines and effective drugs are approved, further reducing the severity of the subsequent cycles. The COVID-19 epidemic gradually wanes in a couple of years (Fig. 2).
Scenario 3: A pandemic becoming endemic. After a partially effective attempt to thwart the first peak through public health interventions, Singapore manages to bring the epidemic under control with considerable lives lost and monetary losses. However, there is a latent reservoir of cases, and small, localized outbreaks continue to occur, with repeated waves complicated by mutated strains imported from other countries. Unfortunately, immunity is not long-lasting and, individuals can be re-infected or experience reactivation of dormant infections. COVID-19 continues to affect the community and burden the health system for a very long time. The pandemic becomes endemic (Fig. 2).
The COVID-19 pandemic is evolving fast with new information about various aspects of transmissibility, symptoms, and severity of disease becoming available with every passing day. Little can be said with certainty. What is now almost certain is that public health interventions do limit the transmission [11]. We need to maintain efforts to keep the transmission in check as much as possible as the risk for any cluster to erupt, especially in high-risk settings, still exists. Two such examples are the outbreaks of COVID-19 in the migrant worker’s dormitories and cases in nursing homes. A considerable number of unlinked cases also exist in the community. These cases can cause the emergence of new clusters. With continued contact tracing, the numbers are declining, albeit very slowly.
In Singapore, we are likely dealing with a prolonged pandemic. Even if the local situation is well controlled, there will be a reservoir of infection in neighboring countries. The aim should be to keep the incidence and mortality low, allowing the healthcare system to continue to function catering to both COVID-19 non-COVID conditions and emergencies. More comprehensive, more accurate point-of-care testing is another target of improvement. Information technology should be more aggressively used to enhance movement tracking, contact tracing and quarantine monitoring like the TraceTogether mobile App and remote tracking of contacts through video calls are some examples [12].
Still, more instances of circuit breakers cannot be ruled out. The frequency and duration of each subsequent circuit breaker will depend upon the success of the previous ones, fatigue of the population, and intensity of virus transmission at that time. The public compliance with the measures is another crucial factor.
Optimizing the healthcare system capacity will help deal with the burden of the more severe COVID-19 cases. In Singapore, converting vacant hospital spaces into beds, upgrading standard beds to higher-level care beds, and upgrading skills of the staff can be considered. In the face of demand beyond capacity, load policies for admission and discharge should be in place to ensure optimum and uniform care provision commensurate with the severity of the illness. Community isolation facilities help manage infectious/potentially infectious patients who do not need hospitalization.
Safe and effective vaccines and drugs would be the ultimate weapons against the virus. It might take months to get these approved. Once available, these will significantly alleviate the biological, psychological, and economic impact of the COVID-19 epidemic. Resistance to vaccines, nevertheless, may pose a challenge.
The course of the global COVID-19 pandemic will also be very much determined by co-operation and collaboration across borders. Public health professionals, clinical, social, and basic science researchers, clinicians and the pharmaceutical industry must work in unison to help achieve a common goal.
Besides the availability of a medicine or vaccine, implementation and fatigue of population to public health measures, and resistance to be vaccinated (once available) are other factors that will contribute towards the pandemic outlook.
A single wave scenario is the least likely one now, given that COVID-19 is now a global pandemic. What is clear is that the current epidemic will not be quick, and it will not be pretty. Singapore, as a nation, has to be prepared for a sustained fight and work across silos and borders, to overcome the pandemic.
REFERENCES
1. Ma J. Coronavirus: China’s first confirmed Covid-19 case traced back to November 17. South China Morning Post [Internet]. 2020 Mar 13 [cited 2020 Dec 8]. Available from: https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-covid-19-case-traced-back.
2. Ministry of Health. Severe acute respiratory syndrome (SARS). Singapore: Ministry of Health; 2003.
3. Seet B. Commentary: why Singapore is better prepared to handle COVID-19 than SARS. Channel News Asia [Internet]. 2020 Mar 17 [cited 2020 Dec 8]. Available from: https://www.channelnewsasia.com/news/commentary/singapore-better-prepared-to-handle-covid-19-than-sars-12535076.
4. Routley N. Infection trajectory: see which countries are flattening their COVID-19 curve 2020. Visual Capitalist [Internet]. 2020 Mar 16 [cited 2020 Dec 8]. Available from: https://www.visualcapitalist.com/infection-trajectory-flattening-the-covid19-curve/.
5. Huang L, Zhang X, Zhang X, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: a prospective contact-tracing study. J Infect 2020;80:e1–13.

6. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020;172:577–82.


7. Yoo JH. The fight against the 2019-nCoV outbreak: an arduous march has just begun. J Korean Med Sci 2020;35:e56.



8. Hu T, Liu Y, Zhao M, Zhuang Q, Xu L, He Q. A comparison of COVID-19, SARS and MERS. PeerJ 2020;8:e9725.



9. Lu L, Zhong W, Bian Z, et al. A comparison of mortality-related risk factors of COVID-19, SARS, and MERS: a systematic review and meta-analysis. J Infect 2020;81:e18–25.

10. Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect 2020;22:69–71.



11. Ng Y, Li Z, Chua YX, et al. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore: January 2-February 29, 2020. MMWR Morb Mortal Wkly Rep 2020;69:307–11.



12. Government Technology Agency. TraceTogther. 1.6.0 ed. Singapore: Ministry of Health; 2020.
-
METRICS

-
- 1 Crossref
- 5,189 View
- 66 Download
- Related articles in J EMS Med