Delayed distal thoracic esophageal perforation secondary to blunt trauma: a case report
Article information
Abstract
Perforation of the esophagus constitutes a true emergency. Esophageal perforation due to blunt trauma results mainly from deceleration injuries, such as high-speed collisions, and it usually affects the distal esophagus. Multiple mechanisms of injury may occur after the esophagus and trachea are compressed between the sternum and the vertebral bodies. Herein, we present the case of a 27-year-old woman who suffered multiple traumas. A chest X-ray was suggestive of left diaphragmatic herniation. However, during the thoracotomy procedure, we discovered a rupture at the gastroesophageal junction. Esophageal perforation should be considered in the differential diagnosis of patients who present to the emergency department with pneumomediastinum, pneumopericardium, or pneumothorax. The difficulty in diagnosing this condition and any delay in treatment can lead to serious complications within 1 to 2 days following the injury. Therefore, it is crucial to diagnose this condition early to prevent thoracic contamination and improve the patient's chances of survival.
INTRODUCTION
Perforation of the esophagus constitutes a true emergency. It most commonly occurs after diagnostic or therapeutic procedures. Spontaneous perforation, also known as Boerhaave syndrome, only makes up 15% of esophageal perforation cases, while foreign bodies account for 14%, and trauma for 10% [1]. Blunt trauma to the esophagus is exceedingly rare, occurring in up to 0.1% of cases [2]. The most frequent cause is high-speed motor vehicle accidents, which usually impact the distal esophagus [3]. The Advanced Trauma Life Support course from the American College of Surgeons points out that esophageal injuries seldom result in death during the initial hours after trauma. However, challenges in diagnosis and postponements in treatment can indeed lead to severe complications 1 to 2 days post-injury. A prompt and accurate diagnosis, coupled with customized treatment, should ensure a positive outcome [4]. In this context, we present a case of delayed distal thoracic esophageal perforation caused by blunt trauma. Informed consent was obtained.
CASE REPORT
A 27-year-old female patient was brought to our emergency department following a motor vehicle accident. She had been riding a motorcycle when she was abruptly struck by a bus on her right side, causing her to fall to the left on January 9, 2018. Her primary symptom was dyspnea, accompanied by complaints of chest pain.
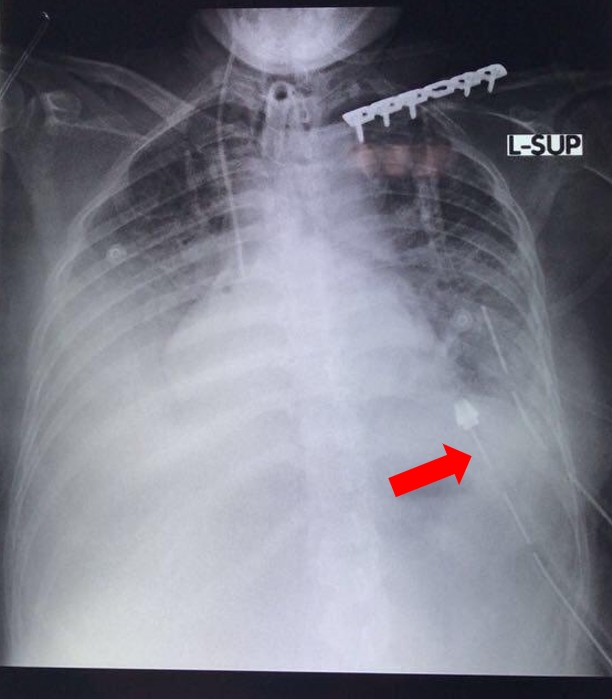
The patient's vital signs were as follows: a blood pressure of 150/90 mmHg, a pulse rate of 148 beats per minute, a respiration rate of 40 breaths per minute, a peripheral pulse oxygen saturation of 96% using a non-rebreathing mask at 15 L per minute, a body temperature of 37.1 °C, and a visual analog pain score of 5–6. The patient's Early Warning Score was 7. Upon examination, it was found that a chest tube had been placed in the left chest. Laboratory results indicated leukocytosis (11,100/µL) and metabolic acidosis (pH 7.332; pCO2 45.4 mmHg; HCO3- 23.5 mmol/L; base excess –2.4 mmol/L). A chest X-ray was performed, which was interpreted as showing a left diaphragmatic herniation (Fig. 1).
The patient underwent a thoracotomy due to left pleural effusion. During the procedure, a rupture was discovered at the gastroesophageal junction. Our cardiothoracic surgeon immediately sought consultation from a digestive surgeon to assist with the operation. The procedure began with the irrigation of the pleural space using normal saline, followed by the primary closure of the esophageal perforation. A T-shaped tube (T-tube) was placed for drainage. A nasogastric tube was inserted through the luminal portion of the T-tube to facilitate gastric decompression and prevent tube migration. A mediastinal chest tube was positioned on the left side of the chest for drainage (Fig 2). Due to hemopneumothorax, a pleural chest tube was also inserted on the right side of the chest. To prevent gastroesophageal reflux and to provide nutrition, a gastrostomy and feeding jejunostomy were performed during this procedure. The patient was treated with broad-spectrum antibiotics and provided with temporary parenteral nutrition. Postoperative care took place in the intensive care unit. The patient remained in the intensive care unit for observation and was discharged after a treatment period of 4 months.
DISCUSSION
Esophageal perforation due to blunt trauma primarily results from deceleration injuries, such as those sustained in a high-speed collision. There can be multiple injury mechanisms following the compression of the esophagus and trachea between the sternum and vertebral bodies. The esophageal wall and adjacent membranous tracheal wall may rupture together; the blood supply could be compromised to the extent of causing necrosis and subsequent perforation. A rapid increase in the esophagus's intraluminal pressure following a cervical spine fracture can lead to esophageal rupture or perforation. However, it is uncommon to see ischemic injuries of the esophageal wall due to the esophagus being bluntly torn from its blood supply, resulting in segmental necrosis. The significant energy required to cause blunt injury to the esophagus almost always results in multiple-system trauma, which can delay recognition [4].
Esophageal perforations often result in symptoms such as pain, fever, difficulty swallowing (dysphagia), and in many cases, respiratory distress. The experienced pain can be located in the chest (thoracic), in the front of the heart (precordial), or in the upper abdomen (epigastric), and it may radiate to the area between the shoulder blades (intrascapular region). If the pleural space, the area surrounding the lungs, becomes contaminated, the patient may experience intense pain on one side of the chest (unilateral pleural pain). The patient's heart rate (tachycardia) is often significantly higher than what would be expected given the degree of fever. The patient may be able to pinpoint the pain in the area around the perforation. Excessive thirst could also be a symptom. Depending on the extent of pleural contamination, the patient may experience difficulty breathing (respiratory distress) [4].
Abnormalities on chest radiography can vary significantly and should not be relied upon for diagnosis. This is because these abnormalities hinge on three factors: (1) the time elapsed between the perforation and the radiographic examination; (2) the location of the perforation; and (3) the condition of the mediastinal pleura. Mediastinal emphysema, a key sign of perforation, requires at least an hour to manifest and is only present in 40% of patients. Swelling of the mediastinum due to edema may not appear for several hours. The location of the perforation can also affect the radiographic results [1]. In 12% to 33% of cases, the radiologic examination may appear normal [4]. However, oral contrast radiographic images are the definitive diagnostic tool. For patients at risk of aspiration (i.e., those suspected of having an impacted foreign body), Gastrografin should be avoided to prevent a severe pulmonary inflammatory and edematous reaction that can occur post-aspiration [5,6].
The management of intrathoracic perforations is based on four principles: (1) elimination of the source of contamination; (2) wide surgical drainage; (3) broad-spectrum antibiotics; and (4) maintenance of adequate nutrition. The specific treatment of esophageal perforation is chosen according to the clinical presentation, which includes the location of the perforation, the degree of soilage, and the patient’s clinical condition [4,7].
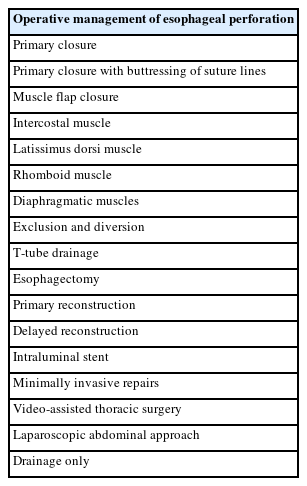
Primary closure of the perforation is the most commonly employed and preferred surgical treatment method (Table 1). The primary objectives of this procedure are to remove all nonviable tissue and to close the esophageal mucosa and muscle in distinct layers. If mucosal closure cannot be achieved in the thoracic esophagus, or if there is insufficient tissue for reinforcement, the perforation can be managed using a T-tube. This converts the perforation into a controlled fistula. A nasogastric tube can be inserted through the luminal portion of the T-tube to assist with gastric decompression and to prevent the tube from migrating. The tube should be secured to the diaphragm in a position that prevents it from eroding into the aorta. Placement of mediastinal and pleural drains should also be considered [5].
After the chest has been closed, both draining gastrostomy and feeding jejunostomy are carried out, either through an open or laparoscopic approach. Gastrostomy is performed to prevent gastroesophageal reflux, while jejunostomy is crucial for maintaining nutrition and promoting healing. Alternatively, a gastrojejunal tube, which serves the dual purpose of decompression and distal feeding, is also considered an acceptable option [5,6,8].
Postoperatively, patients are typically required to fast for a minimum of 5 to 7 days. During this period, their gastrostomy, jejunostomy, or nasojejunal tube should be utilized for enteral nutrition. If enteral access was achieved, the decision to establish central intravenous access and initiate parenteral nutrition hinges on the surgeon's apprehension about a potential postoperative leak. This concern is influenced by the complexity of the repair and the extent of contamination, as well as the patient's initial nutritional status prior to the perforation [5]. Broad-spectrum intravenous antibiotics should be continued for 7 to 10 days postoperatively, but may be continued for longer based on the patient’s clinical status [5].
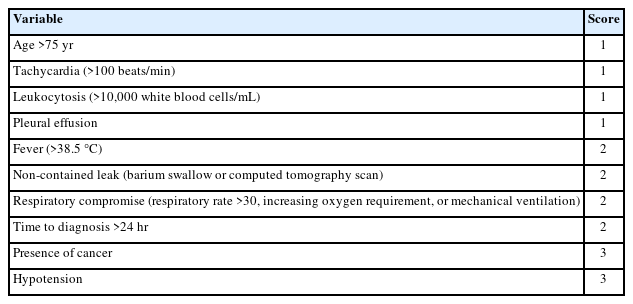
Esophageal perforation is a potentially fatal condition that can result in poor outcomes if the diagnosis is delayed or treatment is inappropriate. Most studies have reported an overall mortality rate ranging from 20% to 30%, often closely linked to the cause of the perforation and the time elapsed between the incident and medical intervention. The Pittsburgh group has proposed a clinical severity score to assess the severity of the injury and predict the likelihood of morbidity and mortality (Tables 2, 3) [9].
Esophageal perforation due to blunt trauma is rare, but it should be included in the differential diagnosis of patients presenting to the emergency department with pneumomediastinum, pneumopericardium, or pneumothorax. In cases of multiple traumas, it is more difficult to diagnose esophageal perforation, so suspicion is first necessary for an early diagnosis. The diagnosis is often determined with contrast esophagography, chest radiography, thoracic computed tomography, or upper gastrointestinal system endoscopy. An early diagnosis is crucial for preventing thoracic contamination and improving survival.
Notes
Funding
None.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Authors’ contributions
Conceptualization: EAT, SW; Data curation: SW, HS; Formal analysis: all authors; Investigation: all authors; Methodology: EAT, SW; Project administration: all authors; Resources: HS; Software: all authors; Supervision: HS; Validation: HS; Visualization: EAT, SW; Writing–original draft: EAT, SW; Writing–review & editing: all authors.