|
 |
- Search
| J EMS Med > Volume 3(1); 2024 > Article |
|
Abstract
Heart failure and decompensated heart failure are conditions with increasing prevalence and incidence worldwide. Sudden cardiac death is a commonly encountered outcome in patients with decompensated heart failure. Early recognition and intervention are the most important protective factors. In this report, we describe a patient who presented to the emergency department with difficulty breathing, using accessory respiratory muscles, and showed a hypoxic and hypertensive course before experiencing respiratory and then cardiac arrest. Early intervention resulted in the return of spontaneous circulation, and the etiology was assessed through bedside ultrasound evaluation of carotid flow time, the thorax, and the inferior vena cava. Upon identifying that cardiac arrest had occurred due to decompensated heart failure, treatment aimed at correcting the etiology was initiated during post-cardiopulmonary resuscitation (CPR) care. The patient achieved full recovery and was discharged. Decompensated heart failure is a significant risk factor for sudden cardiac death. Risk factor control and early intervention are crucial in preventing mortality and morbidity in these patients. This case demonstrates that early intervention and appropriate care following CPR can lead to complete recovery.
Heart failure (HF) occurs when there is a loss of ejection capacity due to structural or functional abnormalities of the heart [1]. Decompensated HF (DHF) occurs when a heart with existing HF is unable to meet the physiological needs of the body. HF has a high prevalence and incidence worldwide, with an incidence of 10% in the population over the age of 70 [2]. A study conducted in 2012 showed that 21.5% of hospital admissions for cardiovascular disease in Brazil were due to HF. Of these admissions, 9.5% resulted in death. Furthermore, 70% of these cases were observed in people over 60 years of age [3]. The causes of cardiac arrest can be attributed to several factors. Post-cardiac arrest care has the potential to reduce early death due to hemodynamic instability and subsequently reduce progressive morbidity and mortality due to multiple organ failure and brain damage [4]. This case describes the post-cardiopulmonary resuscitation (CPR) care of a patient with cardiac arrest due to DHF. Written informed consent was obtained.
An 83-year-old female patient was brought to the emergency department by ambulance (112) with complaints of shortness of breath and dyspnea. On arrival, the patient was in poor general condition with a Glasgow Coma Scale (GCS) score of 8. She exhibited wheezing and use of accessory respiratory muscles during breathing. According to the emergency medical team, the patient, who was in a confused state of consciousness, was brought to the emergency department by her family after experiencing cough and shortness of breath.
Based on the initial assessment, the decision to intubate was made due to the low GCS score and inability to maintain an airway, and a rapid sequence intubation procedure was performed. The initial vital signs were a heart rate of 80 beats per minute, blood pressure of 192/118 mmHg and partial oxygen saturation of 67%.
For rapid sequence intubation, 70 mg of ketamine and 100 mg of rocuronium were administered intravenously (IV) to provide preoxygenation. Due to the patient's short neck and dental structure, this was considered a difficult mask and intubation case. Endotracheal intubation was successfully performed at the third attempt. After intubation, cardiac arrest occurred and CPR was initiated. Asystole was observed as the initial rhythm, and after administration of 1 mg intravenous adrenaline, ventricular fibrillation was detected in the rhythm and pulse check at minute 2, leading to defibrillation. Chest compressions were continued for a further 2 minutes. Return of spontaneous circulation (ROSC) was achieved and pulse-sustained ventricular tachycardia was observed during rhythm monitoring. Synchronized electrical cardioversion was then performed to achieve rate control. After ROSC, the vital signs were observed (Table 1). After CPR application, ROSC was achieved and the patient's condition became stable. During the examination, widespread crackles were heard in the lungs. An electrocardiogram (ECG) showed left bundle branch block, and the heart rate was 113 beats per minute.
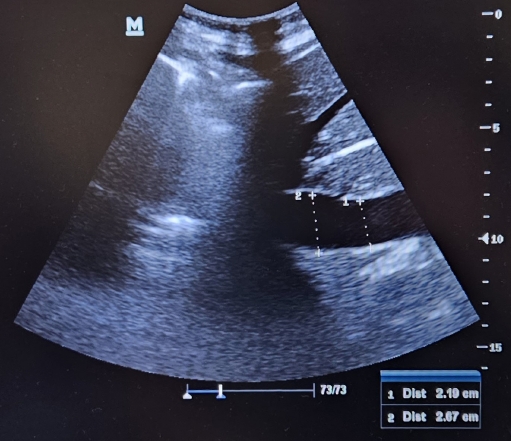
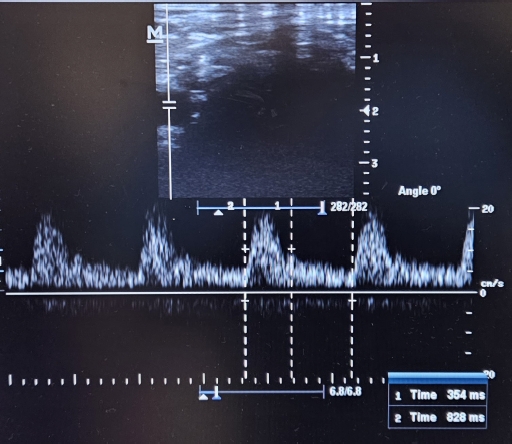
Bedside ultrasonography (USG) was performed to assess the patient. No pericardial effusion was observed on point-of-care USG, B-lines (Fig. 1) were seen on a chest examination, and the diameter of the inferior vena cava (IVC) was measured to be 2.67 cm (Fig. 2). The flow time of the right carotid artery was measured to be 354 ms (Fig. 3). The patient was found to be volume-overloaded. Furosemide (40 mg) was then administered IV as a bolus, followed by a continuous infusion of 20 mg/hr. Nitroglycerin trinitrat ampoules (10 mg/10 mL) were prepared with 100 mL of solution, and an infusion was started at a rate of 20 μg/min.
Once stabilization was achieved, lung imaging was performed. The patient was transferred to the intensive care unit (ICU) for post-CPR care. The patient was extubated one day later. Neurological recovery was observed without any damage.
Transthoracic echocardiography performed at discharge showed an ejection fraction of 40%-45%, indicating moderate to severe mitral regurgitation and moderate tricuspid regurgitation. Following a stay in the ICU, the patient was transferred to the cardiology department and discharged with a full recovery.
Care after CPR includes several components for patients after cardiac arrest. The goals include a comprehensive physical examination, provision of respiratory support, cardiac monitoring, maintenance of body temperature and pain control, which are routine steps in critical care [5]. The differential diagnosis of the patient and analysis of the conditions leading to cardiac arrest include an examination of metabolic values, 12-lead ECG and imaging studies such as X-ray, computed tomography, and USG [6].
In a study investigating the risk of sudden cardiac death in patients with HF, a mortality rate of 15.7% was observed during a 2-year follow-up period. Patients with anemia are at higher risk of sudden cardiac death [7]. In patients with DHF, the timing of treatment initiation is a significant predictor of mortality. Early recognition, initiation of treatment, and follow-up are critical [8].
The flow time, measured non-invasively, can be used to assess hemodynamic status. It is a practical, albeit limited, method of assessing right heart function and pulmonary pressures [9]. HF is manifested by B-line artefacts in lung ultrasound imaging [10]. IVC imaging is important for monitoring patients with DHF, and the observation of IVC collapse of less than 21 mm and greater than 50% collapse is important for discharge planning [11].
In the management of this case, bedside USG was performed to allow early intervention in the patient after ROSC following cardiac arrest. The observed increased flow time, increased IVC diameter and presence of B-lines on chest USG suggested DHF as the underlying etiology of the cardiac arrest. The prompt initiation of treatment for HF and the rapid intervention after the achievement of ROSC led to the patient’s complete recovery.
Table 1.
Vital signs
REFERENCES
1. Bocchi EA, Vilas-Boas F, Perrone S, et al. I Latin American Guidelines for the Assessment and Management of Decompensated Heart Failure. Arq Bras Cardiol 2005;85 Suppl 3:1–48.

2. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2012;14:803–69.


3. Win32, T. 3.0. Morbidade Hospitalar do SUS-por local de internação-Estados [Internet]. 2018 [cited 2023 Jun 2]. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/niuf.def.
4. Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S768–86.


5. Berg KM, Cheng A, Panchal AR, et al. Part 7: systems of care: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020;142(16_suppl_2):S580–604.


6. Mangla A, Daya MR, Gupta S. Post-resuscitation care for survivors of cardiac arrest. Indian Heart J 2014;66(Suppl 1):S105–12.



7. Fukuoka R, Kohsaka S, Shiraishi Y, et al. Sudden cardiac death after acute decompensation in heart failure patients: implications of discharge haemoglobin levels. ESC Heart Fail 2021;8:3917–28.




8. Abdin A, Anker SD, Butler J, et al. ‘Time is prognosis’ in heart failure: time-to-treatment initiation as a modifiable risk factor. ESC Heart Fail 2021;8:4444–53.




9. Alpert JS. The effect of right ventricular dysfunction on left ventricular form and function. Chest 2001;119:1632–3.